Connect with others living with health conditions
- EX Community
- Conversations
- Health Conditions
- Re: COPD: 5 Must Know Updates
- Subscribe to RSS Feed
- Mark Topic as New
- Mark Topic as Read
- Float this Topic for Current User
- Bookmark
- Subscribe
- Mute
- Printer Friendly Page
- Mark as New
- Bookmark
- Subscribe
- Mute
- Subscribe to RSS Feed
- Permalink
- Report Inappropriate Content
COPD: 5 Must Know Updates
Chronic obstructive pulmonary disease (COPD) represents a major burden to global health, and it is a leading cause of morbidity and mortality. Intense research has expanded our knowledge of pathophysiology and therapeutic targets and allowed for the personalization of treatment. The following review provides five disease-related COPD updates.
1. Bronchoscopic Lung Volume Reduction
Bronchoscopic lung volume reduction (BLVR) is accomplished by occluding airways proximal to nonfunctioning, hyperinflated areas of the lung. Several different methods, including endobronchial and intrabronchial valves, coils, and thermal ablative techniques, are used to achieve BLVR.[1] To date, data have shown benefits for symptoms and functional outcomes, but proper patient selection is critical. Head-to-head comparisons between therapies are not available, and although guidelines exist,[2] they're largely based on small trials and expert opinions.
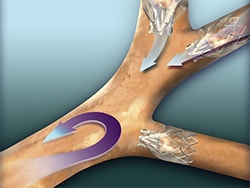
Endobronchial coils and thermal vapor therapies are not approved for use in the United States, but the US Food and Drug Administration (FDA) approved two types of endobronchial valves in 2018: the Zephyr Endobronchial Valve (Pulmonx Corporation; Redwood City, California) and the Spiration Valve System (Olympus Respiratory America; Redmond, Washington). To date, there are more data available on Zephyr valves.[3,4,5] However, in general, both valve types improve symptoms, quality of life, and lung function for patients with COPD.[1] Patients who are most likely to benefit have evidence of air trapping on lung testing (typically a residual volume > 175% on plethysmography) and absence of collateral ventilation (CV) distal to the target area. Typically, CV is assessed using quantitative CT software or the proprietary Chartis System (Pulmonx Corporation). These valves should only be placed at centers that have the appropriate software, equipment, and expertise.[1,2]
2. Tailoring Therapies Using Eosinophil Counts
As we're learning more about COPD phenotypes, we're increasingly able to tailor therapies. Although therapy with inhaled corticosteroids (ICS) is recommended by the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines,[6] its use is controversial. Several studies show an increased risk for pneumonia when patients with COPD use ICS,[7,8,9] and the 2014 WISDOM study found that discontinuing ICS did not affect exacerbation rates in patients using continued triple therapy [long-acting beta-agonist (LABA), long-acting muscarinic antagonist (LAMA), and ICS].[10] Still, other data show a reduction in acute exacerbation of COPD (AECOPD),[9] and patients who continued to receive ICS in the WISDOM study had better lung function than those who did not.
In a recent pro-con debate published in the CHEST journal, two COPD experts debated the use of ICS.[11,12] The authors precisely defined the role that ICS has in disease management, and both recommended using blood eosinophil counts to adjust therapy. Although the relationship between blood eosinophil counts and ICS response tends to be linear, a threshold of 150 (or a differential count of 2%)-300 cells/mm3 has been used as decision point. In addition to assessing the patient's exacerbation rate, both authors recommend using a serum eosinophil count when deciding on the role for ICS in a given patient.
3. Triple-Drug Therapy Via a Single Inhaler
The FDA approved an inhaler that provides triple-drug therapy(LABA/LAMA/ICS) via a single device in 2017. Since that time, several studies have assessed the performance of LABA/LAMA/ICS versus dual therapy with either LABA/LAMA or LABA/ICS. In 2017, the FULFIL trial investigators found that LABA/LAMA/ICS improved lung function and quality of life, and reduced AECOPD compared with LABA/ICS.[13] In 2018, the IMPACT study was published in which researchers found that LABA/LAMA/ICS reduced AECOPD compared with both LABA/ICS and LABA/LAMA.[14] The effect was greatest in those with serum eosinophil counts > 150 cells/mm3. An editorial accompanying the IMPACT study identified several flaws in the design that may have led to the reduction in AECOPD with the triple-drug therapy versus LABA/LAMA.[15] Two additional studies published in 2018 (TRIBUTE and KRONOS) confirmed the results with triple-drug therapy using different active ingredients than those used in IMPACT.[16,17]
The single-inhaler, triple drug therapy results are exciting, but it's not clear how they change patient management. For those who are unconvinced that LABA/LAMA/ICS therapy is superior to LABA/LAMA therapy, the 2018 studies show that triple-drug therapy is a more appropriate treatment, at least in a subgroup of patients. The 2017 GOLD guidelines recommend ICS as add-on therapy to LABA/LAMA for "GOLD group D" patients (those with ongoing symptoms of cough and dyspnea and who experience frequent AECOPD).[6] In the opinion of the authors, the 2018 studies aren't strong enough to alter this recommendation by expanding the indications for ICS.
4. Pulmonary Rehabilitation
It is well established that COPD is associated with breathlessness that affects activity levels. Furthermore, systemic inflammation and corticosteroid use contribute to muscle wasting and weight loss, worsening the functional decline associated with reduced lung function. Medications used to treat COPD target the lungs almost exclusively. All too often, the activity level limits are ignored by physicians.
Exercise is clearly associated with health improvements for the general population and those with COPD.[18] Pulmonary rehabilitation (PR) provides a targeted exercise program designed to optimize activity levels for those with COPD. Its benefits are well established, and for many, if not all, patients with COPD, completion of a PR program will improve functional capabilities far more than is possible with an inhaler. Barriers to referral and compliance have been well documented,[19] and a recently published review clarifies the relationship between poor financial reimbursement and PR availability.[20]Exercise is difficult for these patients, PR takes time, and compliance is poor. However, as physicians, we must be candid with our patients with COPD and emphasize the value from sustained exercise, ideally via a PR program.
5. The Death of Theophylline
Theophylline is one of the oldest COPD medications available. As newer inhalers and targeted therapies have come to market, theophylline has fallen out of favor with clinicians and guidelines. The tight therapeutic window (little difference between therapeutic and supratherapeutic levels) is also an issue, and side effects are common. Still, theophylline remains in the GOLD guidelines,[6] it's inexpensive, and there is evidence for its use and biologic plausibility.[21]
A large, randomized controlled trial published in JAMA studied the impact of low-dose theophylline on COPD outcomes.[22] Of note, the population enrolled had experienced AECOPD, and about 80% were receiving ICS/LABA/LAMA therapy. Adding low-dose theophylline did not reduce the rate of AECOPD compared with placebo. Outside of areas where cost and access to healthcare and drugs is problematic, the use of low-dose theophylline appears to be dead.
https://www.medscape.com/viewarticle/915834_1
Thomas: Please check with your pulmonologist that you are getting the most up to date treatments considering these advances in research. It's your LIFE!
LLAP!
- Mark as New
- Bookmark
- Subscribe
- Mute
- Subscribe to RSS Feed
- Permalink
- Report Inappropriate Content
Good morning Thomas. Thanks for the info. Hope you are healing. I am doing a pilates/yoga class that is pretty wonderful. As always, God bless you my friend.
- Mark as New
- Bookmark
- Subscribe
- Mute
- Subscribe to RSS Feed
- Permalink
- Report Inappropriate Content
Thanks for the update info - and May God continue to bless YOU Thomas in MY Lord Jesus name amen - truthful FACTS to confront the disease of the lungs and to be taught by YOU MY beloved brother who is full of knowledge and wisdom to teach copd survivors to know and be given - NEW knowledge of meds available and each get to choose NEW by EACH individual OWN choice to talk with THEIR OWN DOCTOR - it is THEIR OWN PERSONAL CHOICE for sustaining a NON SMOKER healthier medicine update LIFE style to DO THEIR best for themselves - tough choices YET it's ALL on EACH RECOVERING NICOTINE ADDICT - amen - aah education for EACH individual is the key - so many discoveries of CHOICES- gentle hug❤
- Mark as New
- Bookmark
- Subscribe
- Mute
- Subscribe to RSS Feed
- Permalink
- Report Inappropriate Content
Wow thanks Thomas for sharing this I'm bookmarking it, I'm hoping I'll be able to get a couple of people to read it that's still smoking.
- Mark as New
- Bookmark
- Subscribe
- Mute
- Subscribe to RSS Feed
- Permalink
- Report Inappropriate Content
Thanks for this information, Thomas. I remember when theophylline was widely used, the newer inhalers are effective to a point but the risks of osteoporosis are a real concern. I have used a couple of inhalers that I could not tolerate.
Hope you are feeling much better.
Ellen
